Osteochondrosis usually refers to degenerative changes in any articular cartilage. Thus, this pathological condition can occur in all joints of the musculoskeletal system. However, the most pronounced symptoms, such as headache and headache, as well as heart pain, are noted in the case of cervical osteochondrosis, ie damage to the cartilage tissue between the vertebrae of the cervicobrachial spine.
According to WHO statistics, about 60% of Europeans suffer from osteochondrosis to one degree or another. In men, the disease occurs approximately 10 years earlier than in women. The stricter sex face symptoms around the age of 45. The female half is 55-60 years old, respectively. At the same time, experts are concerned about the continued rejuvenation of this disease. If you do not take timely measures, literally in the next decade the number of 30-year-old patients with osteochondrosis will increase significantly.
Causes of osteochondrosis
Dystrophic changes in the pulp occur for various reasons. The natural aging of cartilage tissue must be put first, which, alas, is an objective and insurmountable circumstance. However, as mentioned above, this disease is getting younger, which is no longer associated with aging, but with other causes.
In young patients, the disease occurs as a result of metabolic disorders, usually associated with improper diet. The abundance of fat and the reduced content of vitamins in food are the reasons why the cartilage literally starts to "starve" and reaches a state of dystrophy.
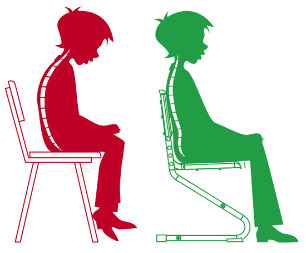
Another provoking factor is physical inactivity. Read the forums where people who have encountered this disease communicate, and you will see that most of them are still relatively young residents of megacities, who are usually engaged in mental work involving a long sitting position. The low motor activity of the cervical vertebrae leads to a loss of elasticity of the cartilage in the intervertebral discs.
As a result of poor nutrition and related metabolic disorders, as well as due to physical inactivity, the pulp begins to degenerate, becoming denser. In the later stages of osteochondrosis, a complication occurs, which manifests itself in the replacement of bone cartilage and thickening of the intervertebral discs. This leads to compression of the nerve roots and blood vessels located here. The participation of the elements of the nervous and vascular system in the pathological process determines the specific course of osteochondrosis.
Specificity of the disease
The difficulty in combating this disease lies in its delayed diagnosis, which is explained by the masking of osteochondrosis in other pathologies. People miss valuable time and do not treat this pathology because they are not aware of its presence. And patients can't be blamed for that. If the pressure jumps, then we treat hypertension. Pierced heart - we go to cardiology. The head hurts regularly and now a person cannot sleep without ibuprofen or analgin. It does not even occur to us that we should visit a neurologist.
In the meantime, just a few visits to a specialist in this profile will allow you to begin the process of restoring the cartilage of each cervical vertebra, which will gradually eliminate false hypertension, as well as suspicions of angina pectoris, and constant headaches and other symptoms. related to the condition of the cervical-shoulder area, the spine, it seems to us, does not appear connected.Early detection of pathology prevents further pulp dystrophy and allows you to treat osteochondrosis at home and on an outpatient basis - without hospitalization. Unfortunately, the lion's share of patients turn to a neurologist already with severe enough lesions of the intervertebral discs - when the neck begins to hurt unbearably.

Diagnostic methods
Diagnosing osteochondrosis is a complex job. The study may take a long time, but its costs are justified, as early treatment of this disease avoids the worst-case scenario - surgery to replace the ossified intervertebral disc, during which the compressed nerve roots and or full-featured implants are released, or ordinary height compensators, which replace a lateral element of the spine. What type of solution is required for a particular patient is determined by the orthopedist after a complete diagnosis.
Since the disease, as mentioned above, is masked, it is first necessary to make sure that the symptoms are not related to problems in other organs. For example, in the case of heart pain, you should undergo a heart examination and confirm the absence of heart disease. A comprehensive diagnosis will allow not only to confirm the suspicion of osteochondrosis, but also to establish the general condition of the body along the way.
The final diagnosis is based on the results of X-ray examination of the cervicobrachial spine in frontal and lateral projections. A more informative method is magnetic resonance imaging (MRI). It allows you to more accurately determine the location of dystrophic changes. Thanks to this, the doctor gets the opportunity to prescribe literally point treatment.
Folk remedies at home
The advantage of osteochondrosis, if the word is used at all in this case, is that the patient can be treated at home without mandatory hospitalization. The course of treatment includes taking special medications and performing exercises from the exercise complex.
The drugs (their types) used to treat osteochondrosis at home are presented in the following table.
| Painkillers | In most cases, these are tablets, sometimes capsules. These remedies are designed to relieve pain in the cervical spine. |
| Anti-inflammatory | Hormonal drugs that stop the inflammatory process as a result of changes in the intervertebral cartilage. It also relieves pain. |
| Chondroprotectors | Medicines containing components for cartilage repair, such as hyaluronic acid. Designed for long-term use. |
| Muscle Relaxants | Means for relaxing muscle tension. These medicines should only be taken under the supervision of a doctor. Limited use due to the large list of contraindications. |
| Outdoors | Ointments, gels and so on. Anti-inflammatory, analgesic and warming agents are used. Before using these tools, you should consult a specialist. |
| Vitamins | Preparations with vitamins that improve the conduction of nerve fibers and the functioning of the peripheral nervous system as a whole. These are B vitamins, as well as A and C. In some cases, vitamin D is prescribed. |
It should be understood that ourenumeration of the types of medicinal products does not give grounds for self-medication. A specific agent with indication of the dose and taking into account the pathogenesis in each case can be prescribed only by a certified neurologist. The pointless adherence to the TV commercial "recommendation" of the best drugs for osteochondrosis is not filled with a cure for this disease, but, on the contrary, with a worsening of the situation. BE CAREFUL!
Injection therapy
In the treatment of osteochondrosis, along with taking pills and applying ointments, injection of drugs is used. There is a wide range of injectable drugs. Treatment courses include all types of injections, including the following:

- subcutaneously;
- intramuscularly;
- intravenously;
- epidural.
Injections are more effective than oral medications and all kinds of folk remedies. Blood flow quickly delivers the agent to the affected area, which explains the rapid healing effect. For example, in an epidural injection, the drugs are injected directly into the spinal cord and take effect immediately.
Vitamins and other maintenance drugs are usually injected subcutaneously. Anti-inflammatory drugs and chondroprotectors are injected intramuscularly. For example,anti-inflammatory drug injections, which are so popular with patients, are injected into muscle tissue. The drugs are injected intravenously to speed up cerebral circulation. This is required in the case of squeezing the overgrown intervertebral discs of the blood vessels through which the blood carries oxygen and nutrients to the brain. Epidural injections are given to block severe pain when other methods of pain relief are ineffective. With this injection, the needle passes between the spinal processes and delivers the anesthetic directly to the spinal cord. This procedure is performed only by a trained professional anesthesiologist.
Injections are completely effective only if you exercise regularly in medical gymnastics. That is, the administration of drugs alone is not enough for the overall treatment of osteochondrosis. Only in combination with exercise therapy is it possible to alleviate the symptoms of the disease and in the future to restore the affected cartilage tissue.
What to do during exacerbations?
Although osteochondrosis of the cervical spine is chronic and more or less unnoticeable for long periods of time, patients sometimes face exacerbations. They occur at different intervals in each patient and can occur unpredictably. During these periods, it is important to take timely measures to prevent significant deterioration.
Exacerbation provocateurs
Exacerbations in osteochondrosis, as in any other disease, do not happen, as they say, suddenly. Acute conditions are usually provoked by the following factors:
- stress;
- non-professional massage;
- meteorological phenomena;
- visit to the thermal bath (sauna);
- excessive physical activity after prolonged physical inactivity.
In women, osteochondrosis often worsens during menstruation. Alcohol abuse is also a powerful provoking factor.
Symptoms of exacerbation
The symptomatology of exacerbations of osteochondrosis in each patient manifests itself differently and is determined by the overall clinical picture of the pathogenesis. For example,cervix and acute headache are noted by all patients, and loss of sensitivity to facial tingling during exacerbations is not felt by all, but still occurs quite often. And, of course, during this period the symptoms of those diseases in which osteochondrosis is masked, worsen. These are heart pain, dizziness, tinnitus, hot flushes and so on. Exacerbations during which inflammation of the cervical vertebrae occurs are especially dangerous.
Exacerbation relief measures
In the period of worsening osteochondrosis, it is necessary to consult your doctor first of all. It is not necessary to ignore this rule, as delays in this matter can do a disservice. The neurologist will assess the patient's condition and recommend steps for an effective and, importantly, safe way out of the crisis.
Injections of painkillers and anti-inflammatory drugs are usually prescribed for acute conditions with osteochondrosis. But gymnastics during this period must be interrupted. On the contrary, the patient must be calm. It is unacceptable to interfere with the neck - it can worsen the condition. It is recommended to transfer the sharpening to a lying position and to fix the head at the same time by placing a roller or at least a rolled sheet under it.An important place to reduce the frequency of exacerbations is their prevention, which comes down to maintaining proper exercise in everyday life.A patient with osteochondrosis should monitor posture, keep his head upright, avoid sudden movements. In wet and cold weather it is necessary to protect the cervical spine from hypothermia. And, of course, you should not forget about medical gymnastics for a minute - you should do it regularly. This is the key to the course of osteochondrosis without exacerbations.
Grade 2 disease
Neurologists distinguish 3 degrees of osteochondrosis - 1st, 2nd and 3rd, respectively. In the lion's share of patients, the disease is registered in the second stage. This is due to the following points. Grade 1 disease is characterized by the appearance of short-term pain in the neck, resembling an electric discharge. In the initial stage, the fibrous ring that holds the central part of the intervertebral disc begins to collapse. The direction for the diagnosis of osteochondrosis of the 1st degree is dilatation of the pupils, which is not related to other phenomena in the body.
The number of patients with grade 1 osteochondrosis is not very large. The disease at this stage is transient and is eliminated (with timely treatment), or quickly passes into the second phase - if the moment is missed. The situation is similar with the number of patients with grade 3 osteochondrosis. It is also small. This is due to the fact that most often doctors manage to start timely treatment and prevent the transition of the pathology from the second stage to the third. The disease of this degree is characterized by symptoms such as acute neck pain that does not subside even after taking painkillers, partial loss of control over the upper extremities, constant dizziness and frequent fainting. Grade 3 osteochondrosis is usually treated with surgery, as drug therapy is often ineffective.
Due to the fact that most patients suffer from osteochondrosis of the 2nd degree, this form of the disease is of the greatest clinical interest and it is in the treatment of the disease at this stage that the greatest experience has been gained. According to statistics, the share of patients with stage II osteochondrosis among all patients with this pathology is about 75%.
The specificity of this form of the disease is its chronic course with short periods of exacerbation.The second degree differs from the first in the continuing reduction of the space between the vertebrae. That is, the intervertebral disc has not yet collapsed, as in the case of the third stage, but it becomes significantly thinner, which leads to pinching of the nerve roots and causes all the classic symptoms of osteochondrosis.
Since grade 2 pathology is the most common, speaking of the treatment of cervical osteochondrosis in general, they suggest the application of therapeutic measures in relation to this particular form of the disease. And they, we repeat, include drug therapy and physiotherapy exercises. Proper treatment allows you to eliminate the disease and prevent its transition to the third stage with almost inevitable surgery to replace the intervertebral discs.
Main symptoms and proper treatment
Osteochondrosis of the cervical spine is a difficult-to-diagnose degenerative lesion of the intervertebral discs. It is most commonly encountered by people aged 45-50 years, but in recent years the pathology has "rejuvenated" and now neurologists often see patients as young as 30 years old.
The difficulty in detecting osteochondrosis is explained by the "simulating" nature of the disease - when it is disguised as other pathologies.The cause of the disease is a deterioration in the elasticity of cartilage tissue, which forms a cushioning pulp between the vertebrae. The cartilage becomes thinner and denser. As a result, the nerve roots are compressed (so-called radicular disorder), which leads to the following symptoms:
- headaches and heart pain;
- high blood pressure;
- decreased sensitivity of the facial area (tingling);
- partial paresis of the upper limbs.
All these symptoms are certainly accompanied by neck pain. Often this pain is mild and does not force the patient to take pain medication. Ignoring the mild pain in the neck, the patient does not sound the alarm for osteochondrosis, but tries to treat other pathologies, such as angina pectoris or hypertension, which he most likely does not have.
Methods of treatment
According to modern approaches, osteochondrosis occurs in waves. Initially it manifests itself in the form of exacerbation (acute period). Then the symptoms weaken and a subacute period occurs. The third stage is remission, which lasts until the next exacerbation. The task for the treatment of osteochondrosis is to quickly stop the acute phase, alleviate the patient's condition in the subacute period and ensure long-term remission.
During the acute and subacute phases, the patient takes painkillers and anti-inflammatory drugs. At these stages, an effective solution is the use of a neck-gauze collar Shants, which gives the head a position in which the neck muscles relax, which eliminates pain. During the period of remission, drug treatment with chondroprotectors, which improve the quality of cartilage tissue, and a set of exercises for exercise are indicated. Exercise is even more important than hyaluronic acid injections because healthy physical activity stimulates the formation of collagen fibers in cartilage in a natural way.
Cervicothoracic type of pathology
Strictly speaking, cervical and thoracic osteochondrosis are two different forms of the disease. However, they are often combined. This is due to the fact that the cervical and thoracic spine are closed to each other, which connects these two types of pathology of the intervertebral discs. That is, in dystrophic changes in the cervical spine, virtually the same disorders are observed in the thoracic region. Therefore, these two forms of the disease are combined, especially since their symptoms are very similar to each other. The main symptom is pain. In cervical osteochondrosis the pain is localized in the neck area, in case of cervicothoracic lesion they are accompanied by pain in the sternum.
Common symptoms include the following:
- facial tingling;
- head and heart pain;
- instability of blood pressure;
- loud tinnitus.
In case of damage to the thoracic vertebrae, the list is supplemented by impaired coordination of movements, activation of osteoarthritis of the shoulder joints, numbness of the hands.
Treatment of the cervical-thoracic spine
Treatment is prescribed after a thorough diagnosis using X-ray or magnetic resonance imaging (MRI). The treatment of osteochondrosis is complex - medication and physiotherapy. Drug therapy includes taking anti-inflammatory and analgesic drugs.An important part of treatment is the use of chondroprotectors, which directly restore cartilage in the intervertebral space. Physiotherapy measures include compresses and the use of all kinds of ointments, as well as physiotherapy exercises.
If osteochondrosis is found in the thoracic spine, professional massage is indicated. The massage effects activate the natural processes of cartilage tissue regeneration. Massage is more effective in eliminating the disease in the thoracic spine than gymnastics, because the spine in this place is not flexible and therefore when performing exercises it is not always possible to ensure a normal range of motion of the individual vertebrae. The masseur, on the other hand, is able to have an accurate effect on a diseased intervertebral disc. Only you need to contact a specialist in spinal massage, who has the appropriate certificate. Also, the masseur must be licensed.
Timely measures to eliminate cervicothoracic osteochondrosis will avoid surgery to replace a damaged intervertebral disc with an endoprosthesis. Early diagnosis of pathology and discipline in outpatient treatment with drugs and folk remedies will save you money. If you have the slightest suspicion of osteochondrosis, consult a neurologist. But better. . .
Be sure to consult your doctor before treating diseases. This will help to take into account individual tolerability, to confirm the diagnosis, to make sure that the treatment is correct and to exclude negative drug interactions. If you use prescriptions without consulting a doctor, it is entirely at your own risk. All information is provided for informational purposes only and is not medical assistance. The entire responsibility for the application lies with you.



































